Current
best practices and rationalistic perspectives in causation-based
prevention, early detection and multidisciplinary treatment
of breast and gastric cancer
|
|
EDITORIAL
Optimizing Lymph Node Dissection for Gastric Cancer ABSTRACT
Although
extended (D2) lymph node dissection is often required for curative
surgery, that is the treatment of choice for gastric cancer, its
therapeutic value has not yet been established. The effect of
lymph node dissection on short-term outcome (morbidity, mortality)
and long-term survival is still highly debated. A preliminary
report of a recently completed Japanese randomized trial (4th
IGCC, 2002), in contrast to the two European randomized trials
available (N Engl J Med 1999;340:908-14, Br J Cancer 1999;79:1522-30),
provides evidence for the safety of extended lymph node dissection
when two conditions are met: experience of surgeon and standardized
pancreas-preserving technique. However, whether D2 dissection,
as compared with limited (D1) dissection, significantly reduces
recurrence-risk and improves survival needs further evidence-based
evaluation. This assessment is very complex and represents the
current challenge of evaluation because several factors including
stage migration confound even randomized comparisons of D1 and
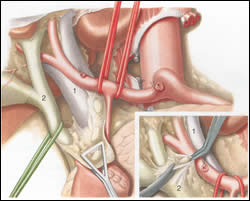
D2 resections. Alternatively, the benefits of D2 dissection can be evaluated on the basis of a recently described concept (Surgery 1998;123:573-8). Key points are the calculations of (1) quantity of lymph nodes dissected by D2 and left behind by D1 dissection (celiac axis/hepatoduodenal ligament). (2) the magnitude of metastatic disease-risk in these level II (N2) nodes that reflects the D1 dissection-attributable risk of residual disease and (3) survival rate of these N2 patients after curative D2 dissection. These calculations (Ann Surg Oncol 2000;7:253-5), which have received little attention by the literature, indicate that 1 additional life would be saved for every 13 patients treated with curative D2 dissection. Furthermore, the benefit of D2 dissection might be greater if micrometastatic disease in level II nodes affect survival but this issue is still controversial. Taken together all these data a decision about the extent of optimal lymph node dissection in the individual patient with gastric cancer can be made. Six
figures clearly show the benefit of D2 vs. D1 dissection from
surgical-oncological point of view. This is the additional fatty-connective
tissue, with containing level II nodes, removed from celiac
axis (superior border of pancreas) and hepatoduodenal ligament
by D2 and left behind by D1 dissection.
Comments
and questions? Please contact us.
|
|